Asthma is one of the most prevalent chronic childhood respiratory conditions, contributing to great losses in quality of life, costs, and morbidity. An estimated 4.9 million children (8.4% of total US children population) suffer from asthma, with 42.9% classified as severe or uncontrolled. Asthma is the second most common reason for pediatric emergency room visits that lead to hospitalization. Asthma not only impairs quality of life but it also contributes significant costs to the healthcare system, particularly for emergency room visits and hospitalizations, which in many cases could be preventable.
What We Do
Medicaid Population Study
Because of limited physician participation in the Medicaid program, many children with asthma rely on Emergency Department care for most of preventable health outcomes. Many children in the Medicaid system do not have access to regular wellness visits, including flu vaccination, and they are rarely seen by specialists. This is particularly critical for controlling asthma. Using retrospective Medicaid claims data, our research spans multiple directions, including deriving a set of baseline measures for asthma care, linking access to outcomes, and identifying trends in care utilization and cost. The end point is to design policy and network interventions to improve health outcomes and access with limited resources.
Access
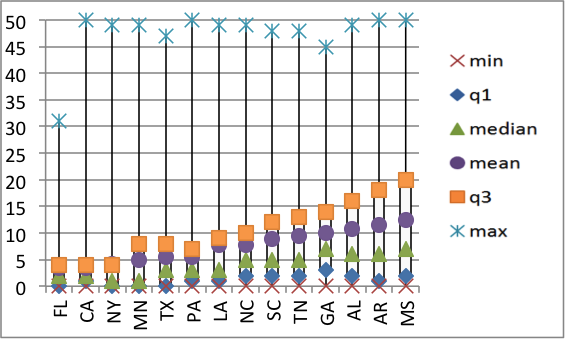
Even though asthma is a common disease among children, access to care for asthma is insufficient and exhibits great disparities. The accompanying figure displays the distribution of the travel distance to access pediatric asthma specialist care across 14 states estimated using our preliminary models. The estimated distances vary significantly between and within states. In this research, we develop a framework for measuring, linking to outcomes and evaluating interventions on spatial accessibility.
Asthma Baseline Metrics
To evaluate the impact of interventions, or to design interventions to have the greatest impact with limited resources, it is useful to develop an asthma baseline. We propose to quantify a set of measures around pediatric asthma for the Medicaid population. Our initial baseline includes elements related to outcomes and costs, for geographical areas and subpopulations within the state of Georgia (called analysis of “small area variations”).
Care Pathways
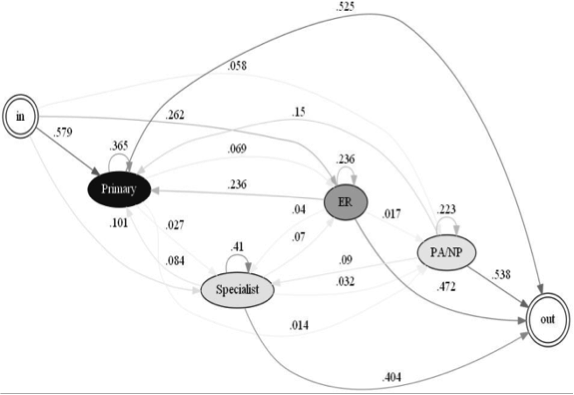
Care for pediatric asthma is complex because of its differential impact depending on several confounding factors including age, provider of care, severity of the condition, access to care, and environment. There are different actions of asthma care, from doing nothing, to obtaining care from a primary care physician or asthma specialist, or simply visiting emergency departments when severe. In this research, our overarching objective is to describe underlying asthma care pathways, where for each pathway we evaluate utilization and cost to suggest potential policy and network interventions.
Publications
Published by the Health Analytics Group
Smith, A., Serban, N., Fitzpatrick, A. (2019), Asthma Prevalence Among Medicaid-enrolled Children, Journal of Allergy and Clinical Immunology: In Practice, 7(4):1207-1213.
Serban, N. (2019). Healthcare System Access: Measurement, Inference and Intervention, John Wiley & Sons, NJ.
Hilton, R., Zheng, Y., Serban, N.(2018) Modeling Heterogeneity in Healthcare Utilization Using Massive Medical Claims Data, Journal of the American Statistical Association, 113(521), 111-121.
Hilton, R., Zheng, Y.R., Fitzpatrick, A., Serban, N. ( 2017) Uncovering Longitudinal Health Care Behaviors for Millions of Medicaid Enrollees: A Multistate Comparison of Pediatric Asthma Utilization, Medical Decision Making, 38(1):107-119.
Garcia, E., N. Serban , J. Swann, and A. Fitzpatrick (2015). “A Study of the Impact of Geographic Access on Severe Health Outcomes for Pediatric Asthma”, Journal of Allergy and Clinical Immunology, featured as New Research Article, 136(6):610-618.
Basole, R.C., Braunstein,M., Kumar,V., Park, H., Kahng, B., Chau, P., Tamersoy, A., Hirsh, D.A., Serban, N. Bost, J., Lesnick, B., Schissel, B.L., Thompson, M. (2014) ``Understanding Variations in Pediatric Asthma Care Processes in the Emergency Department using Visual Analytics", Journal of the American Informatics Association, 22(2):318-23.
Other Publications
Flores, G. F., Abreu, M., et al., (2005). Keeping Children with Asthma Out of Hospitals: Parent’s and Physicians’ Perspectives on How Pediatric Asthma Hospitalizations Can Be Prevented. Pediatrics, Vol. 116, No. 4, 957-865.
Kodner, D. L., Spreeuwenberg, C., (2002). Integrated care: meaning, logic, applications, and implications – a discussion paper. International Journal of Integrated Care, Vol. 2.
Piecoro, L. T., Potoski, M., et al., 2001. Asthma Prevalence, Cost, and Adherence with Expert Guidelines on the Utilization of Health Care Services and Costs in a State Medicaid Population. Health Services Research, Vol. 36, No. 2., 357-371.